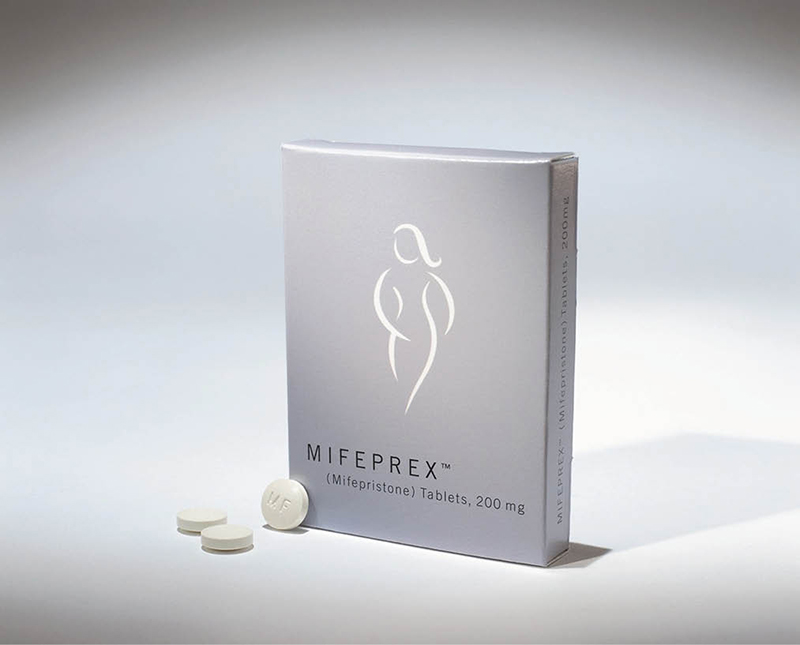
A box of medication used to induce abortion, known generically as mifepristone and by its brand name Mifeprex, is seen in an undated handout photo. (OSV News photo/courtesy Danco Laboratories)
By Maria Wiering
OSV News
More than 20 years ago, Toni McFadden took the abortion pill to end her pregnancy. She was a high school senior, the “good girl” in her family, and she did not want anyone to find out.
She was about seven weeks pregnant when she took the regimen’s first drug — mifepristone — at an abortion clinic. She was sent home to take the second drug — misoprostol — at home. The doctor told her to expect bleeding like a heavy period. When she took the misoprostol, nothing happened. She called the clinic, and was briskly instructed to take a back-up dose she had been given. She did, and there was just a little spotting — but, since she was told the baby was only the “size of a pea,” she thought maybe that was it.
A month-and-a-half later, she was sitting in class when she started to feel “excruciating” pain and began passing blood clots the size of her fist. She realized what was happening, but was unprepared for the pain intensity or blood loss. She called her mother, told her she was experiencing bad menstrual cramping, and went home to sit on the toilet and lay on her bed.
She does not remember how long she bled, or if she saw her baby as she passed it in the toilet. “There’s a lot of trauma with that,” she explained. She does remember laying curled up, in the fetal position.
McFadden, now 43, has become a Christian and pro-life activist. A Pennsylvania native, she continues to share her story amid a national conversation about the availability of “chemical” or “medication” abortion, as well as the protocol some doctors use to interrupt the first pill’s effect, which can save the unborn baby.
“I think people think, ‘Oh it’s just a pill, it’s really easy,’” McFadden told OSV News May 9. “No, there’s something different with this procedure, because with the other procedures, the doctors are doing that to you. With the pill, I took it. Like, I put these pills in my mouth. So, when I had to come to the reality that I took the life of my own child, that hits a little bit different than me being sedated, laying on a table and the doctor took my child.”
In the two decades since McFadden’s abortion, the abortion pill regimen has remained largely the same — a dose of the drug mifepristone followed by misoprostol 24 to 48 hours later — but protocols around it have loosened dramatically, from initially taking place at a clinic under a doctor’s care, to being available by mail after a virtual doctor visit or filling out a form.
In her role as Project Rachel coordinator in the Diocese of Toledo, Ohio, Kerstin Pakka regularly speaks with women seeking healing from abortion. In the past year, she said she has been contacted by an increasing number of women who have had chemical abortions, and they often are looking for help weeks after the abortion, much sooner than the years that pass for many women who have had surgical abortions before they seek out Project Rachel.
Chemical abortion is a “completely different trauma, it’s a completely different experience” from surgical abortion, Pakka said.
“With a chemical abortion at home, you are there usually by yourself and you’re experiencing everything. You’re the one taking the pills, you are the one experiencing the symptoms, and you’re the one who was seeing what happened,” she said. “It’s a very immediate sense of ‘this isn’t just a clump of cells. This isn’t just tissue. This is my child.’”
The abortion pill is prescribed for as late as 12 weeks gestation. By nine weeks, the embryo has visible characteristics — limbs, hands, a face with discernible eyes, nose and ears. Most women who have chemical abortions presumably flush their baby’s body down the toilet, which has been the case for the women Pakka has counseled.
“It definitely adds to the trauma then, that that’s the way they have to dispose of their baby,” she said. For some women she knows, being at home, or in the bathroom or shower, triggers post-abortion trauma.
A lawsuit alleging that the U.S. Food and Drug Administration circumvented its own rules in regulating mifepristone, heard by the U.S. Court of Appeals for the Fifth Circuit in New Orleans May 17, includes a friend-of-the-court brief from women injured by abortion that ends with two pages of the names of women who have had abortions, as well as the names they gave their aborted babies. The brief states, “Surgical abortion is still available for women and less traumatic than chemical abortion because the injury from surgical abortion does not occur in her own home, and does not involve actually seeing the aborted child. … This injury outweighs any harm that will result if this injunction is granted since there is no harm to other women who can still obtain surgical abortions and the injunction is in the public interest.”
Dr. Ingrid Skop, vice president and director of medical affairs for Charlotte Lozier Institute, the research arm of the pro-life organization SBA Pro-Life America, calls foul on some abortion-supporter’s claims that the abortion pill is safer than Tylenol.
“It’s a dishonest comparison,” she said. “They look at the number of Americans who die of Tylenol overdoses, which is about 600 a year, and they compare it to the vastly undercounted deaths that are attributed to abortion,” about two a year, she said. “That comparison fools women into thinking, ‘Oh, I take Tylenol for a headache, and it’s never hurt me. So this chemical abortion must be a similar process,’ but it’s not.”
One survey found 40% of women described the pain as “severe,” said Skop, a board-certified OB-GYN who has retired from private practice but still covers labor and delivery and emergency care at a Texas hospital several times a month.
Even with a doctor’s oversight, it is not safer than surgical abortion, Skop said. From the available data, “it looks like it’s probably about one in 20 women that will have an emergency room visit, and about one in 20 women that will require surgery,” she said.
Experts have interpreted available data differently, with some determining that chemical abortion is relatively safe, and others determining it is not. Skop said that because the FDA does not mandate health care providers to report non-death complications, the data is incomplete, and the studies the FDA cites were done by organizations that describe themselves as committed to readily available abortion.
Skop helped to author a study published in 2021 of post-abortion emergency room use in 17 states from 1999 to 2015. It concluded that “chemical abortion is consistently and progressively associated with more postabortion ER visit morbidity than surgical abortion,” and that “there is also a distinct trend of a growing number of women miscoded as receiving treatment for spontaneous abortion in the ER following a chemical abortion.”
Women who take the abortion pill are unlikely to know when typical bleeding or pain becomes a health emergency, or if they are actually experiencing life-threatening complications from ectopic pregnancy, Skop said. That knowingly puts a burden on emergency room care, she said.
She also is not surprised that more women don’t speak out about a negative chemical abortion experience. She has asked women who experience complications if they want to file a complaint, only to be told they feel they deserve what happened. “They just want to put it away in the back of their mind, and they want to move on,” she said. “But it is a horrible experience, and we really need to try to keep women from having to go down that road.”
As chemical abortion continues to climb as a proportion of overall U.S. abortions, the differences between the experience of chemical and surgical abortion impacts how post-abortive healing ministries such as Project Rachel minister to them, Pakka said.
Women who have taken the abortion pill “feel that they are solely responsible for what happened,” she said. “My job is to show them that they are lovable, that they are loved, that they are worthy of forgiveness of mercy, and that they’re not alone.”
Maria Wiering is senior writer for OSV News.